The Ultimate Guide to Residual Lower Limb Care



Embrace Your Journey: How new amputees can care for their residual limb with love and healthy habits.
At Ottobock.care, we understand that your journey is unique. Taking care of your residual limb is a vital part of your healing and growth, and we're here to guide you every step of the way.
Being proactive to establish healthy habits and routines is essential for your health and mobility. Prosthetic sockets often trap sweat and prevent air from circulating, which creates a paradise for unwanted bacteria. Bacterial and fungal infections can lead to irritated skin, abrasions, and even skin breakdown. Left unchecked, this can cause dangerous infections or ulcerations, ultimately leaving you unable to use your prosthesis and impeding your daily mobility and recovery.
We’ve compiled several tips that can go a long way toward keeping minor problems from turning into something bigger and more dangerous. We advise following the direction of your physician if any of the suggestions stated below differ from their instructions. Please consult with your physician or prosthetist before making any changes in your routine.
Limb Care: Prioritizing Healthy Habits
Your journey starts with understanding how to care for your limb. In the early stages, using a shrinker at night and donning your prosthesis upon waking helps manage swelling—in other words, don’t let your leg hang down often or it will swell. It is advisable to wear your shrinker at night until you and your prosthetist recognize that your limb volume is stable, which could be necessary for up to a year following your amputation.
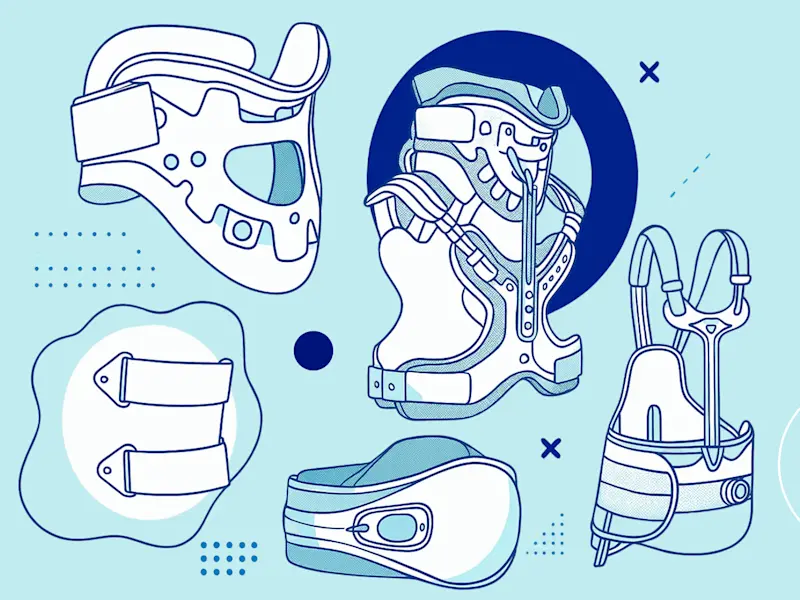
If you don’t have a shrinker, you can alternatively use a Figure-8 wrapping technique on your limb. Please view the figures below for instructions on how to Figure-8 wrap your residual limb. Both above knee and below knee depictions are provided.
Please note that it is not advised to use a shrinker with open wounds, weeping skin areas, arterial insufficiency, acute thrombophlebitis, non-reduced edemas, or non-compensated cardiac insufficiency. Always consult with your prosthetist to ensure shrinker use is a good decision for you.
Sleeping and your residual limb
For below-knee amputees: Never sit or sleep with a pillow under your knee, as this could affect your ability to straighten your knee, which can make walking more difficult and even change how your prosthesis functions.
For above knee amputees: Do not sleep with your limb resting on a pillow, as this could affect your ability to straighten your hip. Sleeping with a pillow between your legs could lengthen your inner-thigh muscle and shorten the outer-thigh muscle, which limits your ability to keep your prosthesis underneath you.
Use your own discretion to find a way to sleep comfortably, and always consult your practitioner for advice and support if you are experiencing issues or discomfort while sleeping.
To support flexibility and movement, daily stretching exercises focused on your knees and hips will go a long way. Thinking back to your physical therapy sessions, use those recommended exercises to make daily activities like walking, and even lying in bed, more comfortable. Unless otherwise directed by your physician or prosthetist, the exercises given to you by your physical therapist should be continued throughout your journey for optimal strength and comfort. They are especially necessary if you have any setbacks that leave you without your prosthesis for any amount of time.
We cannot stress enough how important it is to focus on strength and mobility—without proper care and work, you could experience unnecessary pain while using your device, or even cause the device to not work properly for you.
We recommend working with your physician, therapist, and prosthetist to manage your care as best as possible.
If you’re working with an Ottobock.care clinic, our dedicated practitioners will work closely with your physical therapist to ensure we’re doing everything we can to meet your goals. Ask your prosthetist for recommendations of local physical therapists that have experience working with amputees.
Skin Care: Protecting an Important Barrier
Your skin deserves gentle, precise care as a main barrier to comfort and an effective prosthesis, so let’s dive into an amputee’s skincare routine!
Follow these guidelines to ensure clean, comfortable skin:
Nighttime bathing: For newer amputees, showering or bathing at night eases the fitting of your prosthesis in the morning. Sitting down to bathe or shower with hot water will cause your limb to swell.
Daily washes: Wash your limb with mild soap and water every day (more often if you sweat more), and pat it dry with a soft towel. Ensure it dries completely to avoid fungal or bacterial infections. You want soap that is non-scented and non-antimicrobial as these two factors introduce chemicals to the skin that can cause irritation. Dove is a good option for mild soap.
Skin check: Check for skin breakdown at least twice a day. This is especially important for folks with diabetes. Pro-tip: Use a mirror if you can’t see the end of your residual limb!
Lotions and creams: Softening cream should only be used when the skin is extremely dry and at the risk of cracking. Let your skin absorb the product before putting on your liner or prosthesis.
Avoid extreme heat: Avoid exposure to hot water or direct sunlight so your skin doesn’t blister. Remember, your limb is covered all the time, so diligently use sunscreen if it could be exposed for an extended period of time.
Pay attention: If you experience reduced or no sensation in your limb, check your limb more frequently for any changes.
Important DON’TS to remember for your skin:
DON’T use talcum powder/baby powder, as it can ball up and cause an abrasion. If you must use powder, cornstarch is preferred.
DON’T use alcohol or other unknown chemicals and creams on your limb.
DON’T use any products (lotions, soaps, etc.) with fragrances.
DON’T shave your residual limb, as this could cause infections from ingrown hairs.
Always work with your prosthetist if you are experiencing any skin issues that might be caused by an improper socket fit. Bring in your physician as needed if an infection pops up so you can treat it early. It is not advisable to continue using your prosthesis if you are experiencing any sort of skin breakdown on your residual limb. Take some time away from using your device, use a wheelchair or crutches for daily activities, and ensure you are getting proper exercise and movement in so you’re ready to get back to your prosthesis!
Skin Inspection: Your Daily Wellness Ritual
Regular inspection of your skin is more than a routine; it's a daily ritual that keeps you in tune with your body (especially in your first few months with a prosthesis). If anything looks out of the ordinary, document it and immediately report this to your prosthetist.
What should be considered “out of the ordinary,” you ask? Great question! Check your limb for red pressure patches that last for 10 minutes or more after you remove your prosthesis. These may be a sign that something is off!
While redness is often normal after using your prosthesis, we recommend a Blanch Test if you’re unsure if something is normal/abnormal:
Simply (and gently) push your finger into an area of redness.
If the area immediately turns a lighter color, this is normal.
If the area doesn’t change to a lighter color, this is abnormal.
If the area takes several minutes to return to the original color, this is abnormal.
A red spot that turns into an ulcer can lead to weeks without being able to use your prosthesis, which no one wants for you! If you notice redness persisting despite adjustments like sock ply changes, avoid using your prosthesis and consult your physician as soon as you can.
It’s easy to forget doing these small things for yourself when life gets moving really fast, but we want to remind you that taking the time to prioritize a healthy habit like checking your residual limb skin can save you time, money, and much larger inconvenience later down the line. Baking this into your daily routine is key!
Facing Challenges: Dealing with Possible Infections
Careful attention to the hygiene of your residual limb should be an ongoing activity—not just immediately following amputation surgery. Especially if you are using sockets and liners on a regular basis, making your skin more prone to breakdown and infections.
Should you encounter skin issues that lead to an infection, your physician or prosthetist is here to guide you. Any wound from amputation, surgery, or seemingly harmless scratch is at risk for infection when not properly protected and cleaned. It can happen to anyone at any point in their journey without forming the health habits and routines we’ve outlined so far. Whether you are experiencing the signs and/or symptoms described below, if you are uncertain about the condition of the skin on your residual limb, please seek the appropriate medical attention to get your questions answered.
Some signs you could be experiencing an infection:
Tenderness or pain around the wound
Wound feels warm or hot
Fever/chills
Sudden increase in pain
Lingering redness
Red lines running up the limb from the wound
Swelling around the wound or in your limb
Wound discoloration and sustained drainage
Symptoms that require emergency attention:
Circulation decreases
Whole extremity feels cool/cold
Wound area smells bad
Swollen glands in groin or armpits
Wound has thick brown/grey drainage
Skin around the wound turns black
It is important to act early if you’re experiencing anything on the lists above. Work with your healthcare provider to determine the best course of action to treat your infection. Often, you will be prescribed antibiotics, and it is key to always finish the entire prescription even if it appears to have cleared up.
Movement in Medicine: Embracing an Active Life
It is so important to prioritize your whole self: body, mind, and spirit. For both physical and mental well-being, we encourage you to stick to physical therapy routines, with a PT or simply at home, as well as finding activities that you truly enjoy participating in. You can work with your prosthetist or practitioner to determine what movement would be the most fulfilling for you. Continuous use and practice with your device during activities you love will make you more confident and comfortable with your prosthesis.
These are some of Ottobock.care patients’ favorite ways to stay active and social:
Adaptive yoga
Wheelchair basketball
Hiking / walking groups
Cycling (indoor and outdoor)
Swim fitness classes
Adaptive horseback riding
Running
Golf
Staying inactive or creating unbalanced eating habits can lead to weight changes that might affect the functionality of your prosthesis. Even slight fluctuations in weight affect the fit of your device, so we recommend trying to maintain the weight you were when you were fit for a prosthesis. If you plan on making a significant change in your weight, work with your prosthetist to prepare for device adjustments.
We understand that insurance coverage for sports prostheses is not the easiest task to manage, and often results in denials. We are constantly working with partners across the country to advocate for legislation that makes coverage and access to sports prostheses more widespread in public and private health insurances. Recently, advocates from across the O&P industry joined forces for 28x28: A mission to drive legislation for prosthetic component coverage across the country. If you would like to learn more about these efforts or learn how to reach out to your state representatives, click here.
Activate Yourself: Prioritize Self Care
We’re big advocates of self-care here at Ottobock.care (it’s kind of in the name!), and want to remind you that creating healthy habits around your residual limb is just as important as making time for that at-home spa day (or whatever your self-care might look like). Your well-being is worth the time and dedication it takes to form daily, weekly, and monthly routines.
While we’ve outlined a handful of ways to care for your residual limb here, we always recommend working with your prosthetist, physician, and physical therapist on the best solutions for your specific needs and goals. No one knows you better than your doctors!
Get a Consultation
Are you ready to take the next step towards improved mobility and comfort? Find an orthotics and prosthetics clinic near you and schedule your appointment today!